Post-doctoral Fellowship
Human Genetics Research
National Cancer Institute
2004

James G. Taylor VI, M.D., is a professor of microbiology who serves as Director of the Center for Sickle Cell Disease at Howard University. A board-certified pediatric hematologist/oncologist, Taylor earned his medical degree from the Medical College of Wisconsin, completed his residency in pediatrics at Washington University in St. Louis, and pursued advanced fellowships in pediatric hematology/oncology and genetics research at Johns Hopkins University and the National Institutes of Health (NIH). His academic training, including postdoctoral fellowships in vascular medicine and genomics at the NIH, positioned him to become a national leader in translational research on sickle cell disease.
Taylor’s clinical and research career has focused on the genetic and physiological underpinnings of pain in sickle cell anemia, particularly within African American populations. He has led groundbreaking studies on pain phenotyping, genetic admixture, and central sensitization in sickle cell disease, significantly advancing understanding of disease complications and informing more precise, personalized approaches to care. As director of a center that serves more than 350 adult sickle cell patients, Taylor oversees a multidisciplinary team of clinicians and scientists, helping bridge research and clinical care to reduce health disparities in hematologic disorders.
With prior roles at Johns Hopkins Hospital and the NIH, Dr. Taylor has received numerous honors, including the NIH Top Science Advance award and citations from the City of New York for his contributions to sickle cell advocacy. His scholarly output spans high-impact journals, and he has held influential roles on grant review panels, editorial boards, and advisory committees. Through his leadership at Howard University and as a co-investigator with the Center for Hemoglobin Research in Minorities (CHaRM), Taylor continues to champion equitable, research-driven solutions for patients historically underserved by the healthcare system.
Human Genetics Research
National Cancer Institute
2004
Pediatric Hematology/Oncology
Johns Hopkins University School of Medicine/NIH
2001
Pediatrics
Washington University, St. Louis
1998
Medicine
Medical College of Wisconsin
1995
Biology
Creighton University
1991
Thalassemias; Hemoglobinopathies; Adult Acute Lymphoblastic Leukemia; Myelodysplastic Syndromes; Non-malignant Hematology Board Review
P50 HL118006, NHLBI/NIH: Center for Hemoglobin Research in Minorities (CHarM)
Taylor, Robert E. (PI)
Role: Co-Investigator
10% effort (2017)
Faculty start-up Award (2017-2019): Howard University College of Medicine (Medicine) and Center for Sickle Cell Disease
Translational analysis of mechanisms of pain in sickle cell disease
Role: PI
Pfizer
RESET clinical trial
Role: PI
Read: Diverse: Issues in Higher Education | Nobel Prize Spotlights Sickle Cell’s Disproportionate Impact on African Americans
Read: World Health Organization | Centre of excellence brings hope for sickle cell patients in Congo Republic
Antiviral response and HIV-1 inhibition in sickle cell disease
Sickle cell disease (SCD) is characterized by hemolysis, vaso-occlusion, and ischemia. HIV-1 infection was previously shown to be suppressed in SCD PBMCs. Here, we report that HIV-1 suppression is attributed to the increased expression of iron, hypoxia, and interferon-induced innate antiviral factors.
Renal manifestations are the most common complications of sickle cell disease (SCD). Renal disease starts during childhood and progresses further in adults.1 Approximately 30% of patients with SCD develop chronic kidney disease (CKD), and 14% to 18% of them progress to end-stage kidney disease. Thus, there is an urgent need to find specific biomarkers for the early detection of CKD in patients with SCD.
Sickle-cell disease, a genetic condition with a high prevalence in sub-Saharan Africa, is transmitted in an autosomal recessive mode. Its screening during pregnancy makes it possible to identify carriers of the S gene which constitute a risk for the unborn child. In order to promote the use of immuno-chromatographic tests, we have set ourselves the task of establishing the epidemiological profile and determining the Emmel test performance.
The gut microbiome in sickle cell disease: Characterization and potential implications
Sickle Cell Disease (SCD) is an inherited blood disorder that leads to hemolytic anemia, pain, organ damage and early mortality. It is characterized by polymerized deoxygenated hemoglobin, rigid sickle red blood cells and vaso-occlusive crises (VOC). Recurrent hypoxia-reperfusion injury in the gut of SCD patients could increase tissue injury, permeability, and bacterial translocation. In this context, the gut microbiome, a major player in health and disease, might have significant impact. This study sought to characterize the gut microbiome in SCD.
Chronic kidney disease (CKD) strongly contributes to morbidity and mortality in ageing sickle cell disease (SCD) patients.1 Biomarkers for early stage CKD, such as proteinuria, microalbuminuria and reduced glomerular filtration rate (GFR), are difficult to detect in SCD patients because of a urine concentration defect. Thus, new biomarkers, which reflect the unique renal pathology of SCA-associated CKD, are needed for early detection and treatment.


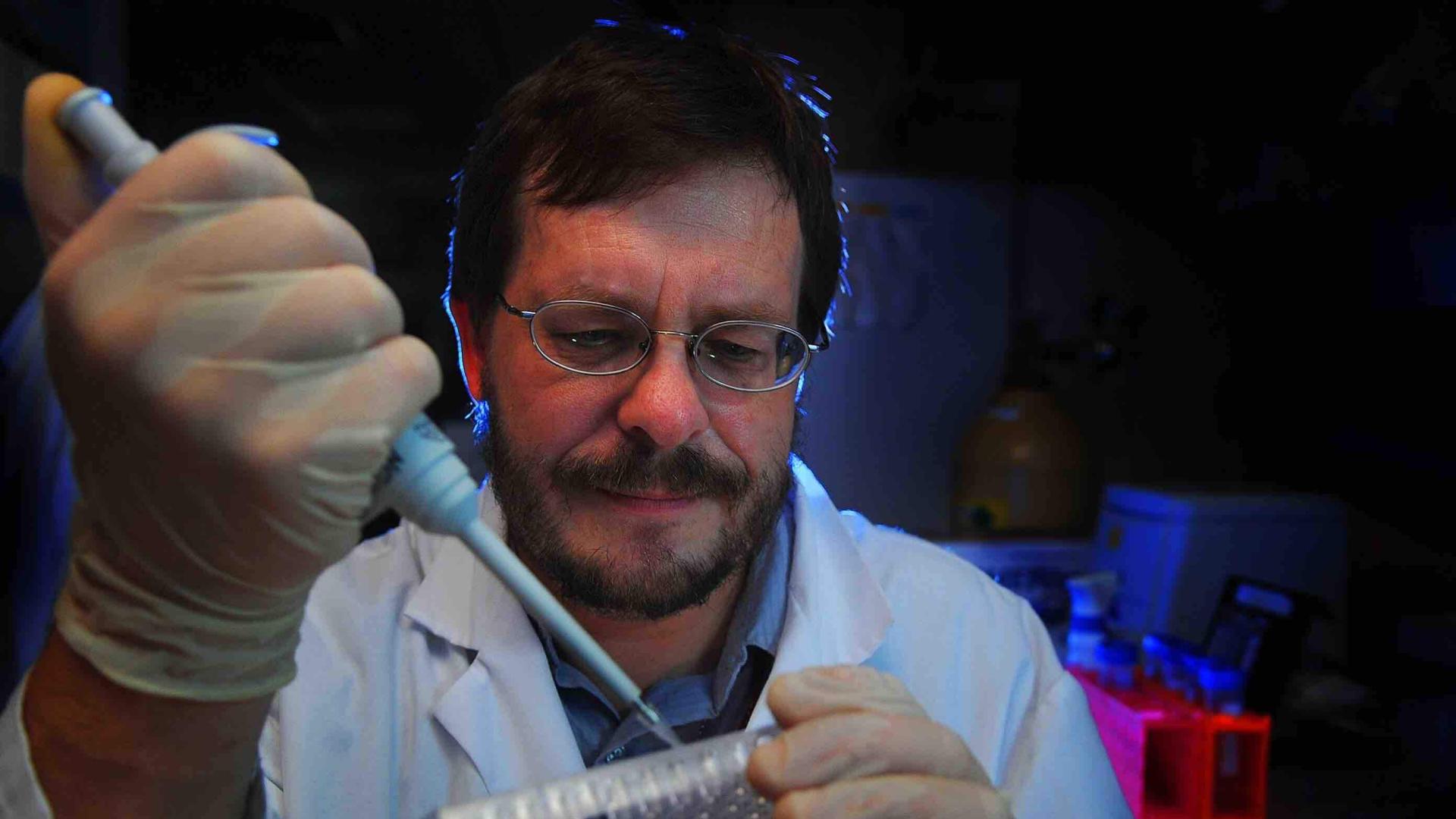


CGTN's Frances Kuo talks with Dr. James Taylor, director of the Center for Sickle Cell Disease at Howard University, about international collaboration in fighting the disease.